Share this
COVID-19 Tests? Consider a Finger-Prick Instead of a Regular Blood Draw
by Neoteryx Microsampling on April 29,2020
 “COVID-19 testing is top-of-mind for every researcher around the world at present, and effective testing is an important part of every coronavirus pandemic safety plan. Testing can potentially be done on a large scale and at home by collecting blood following a finger prick," says toxicologist Christophe Stove, PharmD, PhD, Ghent University, Belgium.
“COVID-19 testing is top-of-mind for every researcher around the world at present, and effective testing is an important part of every coronavirus pandemic safety plan. Testing can potentially be done on a large scale and at home by collecting blood following a finger prick," says toxicologist Christophe Stove, PharmD, PhD, Ghent University, Belgium.
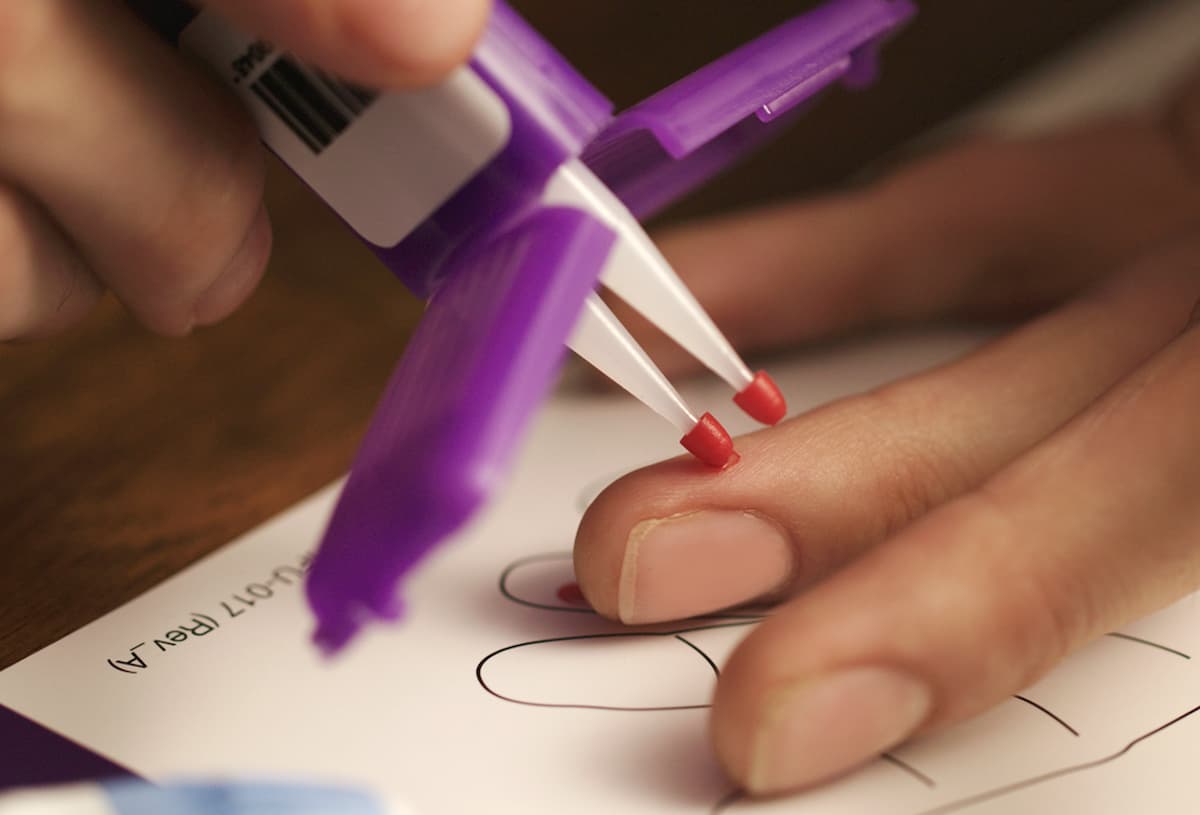
Analysis of a blood drop taken after a small finger-stick: the vast majority of us have already (unknowingly) experienced this type of blood draw just after birth via the heel prick used for newborn screening to detect a number of birth defects. This type of blood draw is also a daily routine for many diabetes patients.
So much information can be gathered from a drop of dried blood. At Ghent University, we routinely perform analysis of dried blood samples to check for the presence of a marker indicating how much alcohol an individual has consumed in the past month. Additionally, a number of Dutch laboratories analyze drug concentrations in dried blood samples. These samples come from patients who have undergone an organ transplant and require lifelong follow-up. They are taking therapeutic drugs to ensure their bodies don’t reject their new organs, and therapeutic drug monitoring (TDM) is necessary to guard against toxicity. These patients can collect their own blood samples at home and send their samples to the hospital.
At-home blood collection has become more widely used during the current COVID-19 stay-at-home measures. To reduce risks of exposure to the coronavirus, in-person visits to a doctor or hospital for a blood draw are rapidly being replaced by at-home blood collection that the patient can manage himself.
With plans to loosen the stay-at-home measures emerging, with the possibility of another coronavirus outbreak in future, and with more extensive testing of (parts of) the population becoming more prominent on the agenda, the question arises: Can effective serology tests be carried out using a drop of dried blood? The answer is “yes,” though it is important to emphasize that these serology tests are not intended to detect the actual virus. For those types of tests, a nose or throat swab is used. The main purpose of a serology test is to check for the presence of antibodies in the blood, as a sign of past infection.
At-Home Blood Collection Gathers Momentum
Blood microsampling and analysis of dried blood drops using at-home specimen collection and shipment to a laboratory has been widely explored over the past 10 years. This is an alternative option we have been using in our lab in addition to, or as a substitute for, conventional blood sampling. We have been using Mitra® microsampling devices from Neoteryx, for example, to explore the possibility of therapeutic drug monitoring of patients. For many applications it has already been demonstrated that reliable lab results can be obtained in this way. We just have to make sure that patients follow instructions for correct sampling. There are also a number of points to consider in regard to the use of remotely collected blood samples in the laboratory.
Soon, blood collected from tens of thousands of people may need to be analyzed, perhaps even several times per person. For this reason, a finger-prick method in a patient-friendly at-home collection kit can be an important advantage. The current situation may provide momentum for the at-home blood sampling industry. After all, contact with a doctor or other medical professional for blood draws can be seen as an additional burden to the healthcare community. Clinic-based blood draws can tax our already overworked healthcare workers, especially since in-person blood draws now also require extra precautions at each visit. This seems an unnecessary burden and risk for a simple blood collection event that could be patient-managed at home.
Moreover, the anticipated scale on which testing may need to be carried out is also an important factor to consider. If a simple finger-prick can be used instead of a conventional blood draw to collect blood samples from tens of thousands of people—perhaps multiple times per person—the use of at-home blood collection kits could be a significant benefit.
High-Quality Blood Samples Are Critical for Antibody Testing
A critical point with a strategy to roll out more at-home blood collection is that no concessions should be made on the quality of the result. After all, reliable data can only be gathered when both the blood sample and testing methods are of good quality.
As far as sampling is concerned, successful examples are available. Last year, in light of “Tournée Minérale,” an initiative in which persons that normally do drink alcohol stay sober for one month, our laboratory carried out a study in which hundreds of persons collected drops of blood at home through the month of February. Instead of sampling their drops of blood onto a piece of paper, as with traditional dried blood sample (DBS) cards, they did this using a small device, a Mitra microsampler, with an absorbent tip. The tip is designed with VAMS™ technology to absorb an exact amount of blood.
Since some of the participants in our study took two samples at home, at the same time, we were also able to demonstrate that the variation from sampling to analysis was very acceptable. This shows that, provided that suitable instructions are provided, correct sampling at home is actually possible, even by people who have never taken such a sample using the finger-prick method. In addition, a simple visual check is possible to make sure the samples meet predefined quality requirements.
The dried blood samples obtained with Mitra Blood Collection Kits can safely be sent by post to a laboratory in a plastic bag in an envelope. In the context of COVID-19, distribution of these blood sampling kits could be performed by pharmacies, whereby the pharmacist could provide the kits, with information regarding correct sampling, to the person who will collect their blood at home.
It is important to note that any family member at home can assist with blood sampling by fingerstick, even if they have minimal experience. The at-home blood collection is easy to do, which makes it possible for a family member to assist a person who cannot perform a fingerstick him/herself (i.e., children, the elderly or disabled). Once enclosed in the collection kit, the dried blood samples can be safely sent in a sealed plastic bag that goes inside an envelope. The packaged sample can be mailed to a laboratory, where the analysis of the blood sample can take place.
Lab Methods to Consider for Analysis of Dried Blood Samples
There are a number of things to take into account for the actual analysis and interpretation of the result. First, the determination is made in blood instead of serum (the liquid fraction in the blood in which the red blood cells are located). In addition, since dried blood is used, an adjustment in the sample preparation procedure is also necessary, since the dried sample of blood must be dissolved again before the analysis can be carried out. This can be done in a very simple way.
A number of laboratory tests will require an adjustment in their implementation. Ideally, there is a conversion from a blood to serum concentration (in which the determination is done by default). Procedures are available for this. There is, of course, the limited sample volume to consider, which implies that the test to be used will have to be sufficiently sensitive.
Specifically, only about 10 µl of blood is taken from the sample, which corresponds to a small drop (only one hundredth of 1 milliliter). The sensitivity factor will largely determine the choice of the laboratory test: after all, not every commercially available test will be able to achieve the desired sensitivity based on such a small volume of blood. In addition, the intrinsic quality requirements of the test must not be compromised and sufficient tests must be available.
SARS-CoV-2 Antibody Testing
For researchers analyzing blood samples for antibodies, there is still the challenge of interpreting the result. For the time being, it can only be determined from a positive result (showing the presence of antibodies to coronavirus) that someone is (or has been) positive for SARS-CoV-2, and has therefore gone through or is going through an infection. It is currently not clear which "titer" or what level of antibodies is needed to provide protection against another infection in future. It is also currently unclear to what degree or for how long a given titer will provide protection against a subsequent infection.
These questions have nothing to do with the test itself. They are also independent of how the result was obtained (by classical determination in serum or via a dried blood drop).
The feasibility of the determination of antibodies in a drop of dried blood is supported by successful examples from the scientific literature. In addition, a number of things highlight the potential of dried blood drops to detect a past infection with SARS-CoV-2.
For example, laboratory tests are currently available that are being used for this purpose; whether they are good enough has yet to be independently evaluated. A serology study using the Mitra microsamplers from Neoteryx was also recently launched in the United States by researchers at the National Institutes of Health (NIH). The NIH study will determine the presence of antibodies in a cohort of 10,000 volunteers via a drop of dried blood.
This news post is curated content. The Dutch-language version was written by Christophe Stove, PharmD, PhD, University of Ghent, Belgium. The English translation and edits were provided by Neoteryx, whose editorial staff apologizes for any inaccuracies in the English translation. View the original document from University of Gent here.
For more information about remote microsampling for COVID-19 studies, click below:

Share this
- Microsampling (41)
- Industry News, Microsampling News (37)
- Mitra® Device (34)
- Company Press Release, Product Press Release (22)
- Research, Remote Research (18)
- Infectious Disease, Vaccines, COVID-19 (15)
- Clinical Trials, Clinical Research (14)
- Biomonitoring, Health, Wellness (10)
- Blood Microsampling, Serology (10)
- Decentralized Clinical Trial (DCT) (8)
- Omics, Multi-Omics (7)
- Venipuncture Alternative (6)
- Skin Microsampling, Microbiopsy (5)
- Harpera Device (3)
- Specimen Collection (3)
- Toxicology, Doping, Drug/Alcohol Monitoring, PEth (3)
- Pharmaceuticals, Drug Development (2)
- Therapeutic Drug Monitoring, TDM (2)
- Antibodies, MAbs (1)
- Environmental Toxins, Exposures (1)
- Preclinical Research, Animal Studies (1)
- hemaPEN® Device (1)
- February 2026 (1)
- January 2026 (1)
- December 2025 (1)
- May 2025 (1)
- April 2025 (1)
- February 2025 (4)
- September 2024 (1)
- August 2024 (1)
- May 2024 (2)
- January 2024 (1)
- December 2023 (2)
- November 2023 (3)
- October 2023 (2)
- September 2023 (1)
- August 2023 (3)
- July 2023 (3)
- June 2023 (1)
- May 2023 (2)
- April 2023 (1)
- March 2023 (2)
- February 2023 (1)
- January 2023 (2)
- December 2022 (1)
- November 2022 (1)
- October 2022 (2)
- August 2022 (1)
- April 2022 (1)
- February 2022 (1)
- January 2022 (1)
- December 2021 (1)
- November 2021 (1)
- October 2021 (2)
- September 2021 (1)
- August 2021 (2)
- July 2021 (2)
- June 2021 (2)
- April 2021 (1)
- March 2021 (2)
- February 2021 (1)
- January 2021 (1)
- December 2020 (1)
- November 2020 (1)
- October 2020 (1)
- September 2020 (2)
- August 2020 (3)
- July 2020 (3)
- June 2020 (2)
- May 2020 (1)
- April 2020 (3)
- October 2019 (1)
- March 2019 (1)
- January 2019 (1)
- November 2018 (1)
- August 2018 (1)
- July 2018 (1)
- June 2017 (1)
- April 2017 (1)
- March 2017 (1)
- February 2017 (1)
- May 2016 (1)
- December 2015 (1)
- October 2015 (1)
- August 2015 (1)
- August 2014 (1)
- July 2014 (1)

Comments (5)