Share this
Podcast: microsampling in proteomics & multi-center studies
by Neoteryx Microsampling on Jan 29, 2024 9:00:00 AM

For this episode of the Microsamplify Podcast, our Microsampling Technical Director James Rudge, PhD, interviews Stephen Pennington, BSc, PhD, a research scientist with expertise in using mass spectrometry to measure and characterize proteins.
Since the first use of the term Proteome Analysis, now Proteomics, Professor Pennington has spoken and published on the subject widely. Steve is professor of proteomics at University College Dublin, president of the British Society of Proteome Research, and past President of the Human Proteome Organization (HUPO), which recently awarded him a distinguished service award.
Steve has filed a number of patents, served as a consultant to several companies, and in 2017 he founded the diagnostics data company Atturos. Prof. Pennington is an advocate of microsampling in omics and other studies, which he uses in his research collaborations, including a recent multi-center European research project called HIPPOCRATES that aims to improve outcomes for people with Psoriatic Arthritis.
Neoteryx: Hello Professor Pennington, and welcome to the Microsamplify Podcast from Neoteryx. Thanks for taking the time to speak with us about proteomics and microsampling, and how those tie together in your work.
Dr. Pennington: Thank you, James. It’s a real pleasure to join you on this Neoteryx podcast, and I very much look forward to speaking with you.
Neoteryx: You’ve dedicated much of your career to proteomics, so I’d like to start things off by asking you to tell us more about what drives your interest in proteomics and how you view the importance of it in future science and personalized healthcare?
Dr. Pennington: Early in my career, while I was doing a PhD on lipid metabolism, of all things, at the University of Cambridge, I became fascinated with intra-cellular signaling — in particular, how protein receptors on the surface of cells could convey signals rapidly to the nucleus. 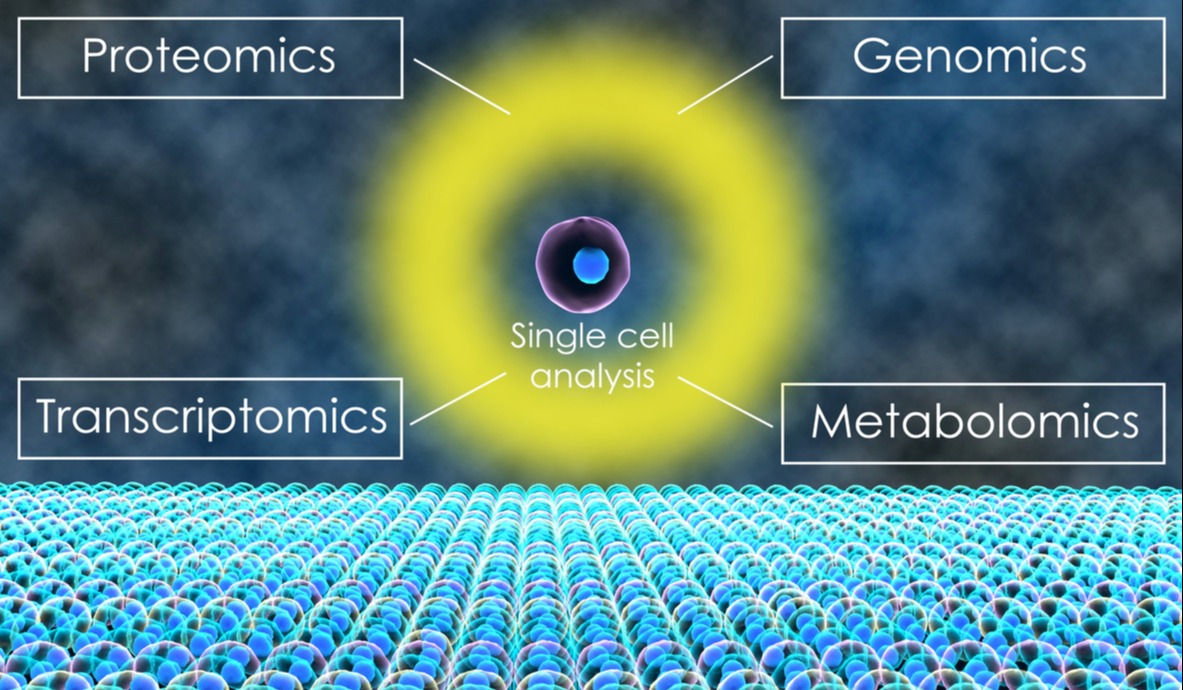 It became apparent that, for some receptor signaling pathways, this may be achieved by the movement of proteins from the cytoplasm of the cell into the nucleus. It was at that stage we were introduced to the technique of 2D gel electrophoresis to look for proteins that translocate.
It became apparent that, for some receptor signaling pathways, this may be achieved by the movement of proteins from the cytoplasm of the cell into the nucleus. It was at that stage we were introduced to the technique of 2D gel electrophoresis to look for proteins that translocate.
And that subsequently led us into the world of proteomics. Since then, it has become apparent that – and I think it should be apparent to all – proteins are the key molecules that execute cell function.
So, to understand health and disease, we need to understand how proteins function. Needless to say, but I’ll say it anyway, in all their diversity proteins continue to fascinate and enthrall me…all aspects of them. In recent years, it has also become apparent that studying proteins on a genome scale (proteomics) has a really important potential impact on the future of personalized healthcare. In the case of Atturos, using blood proteins as biomarkers.
Neoteryx: In recent years, the use of dried serum spots has gained interest in the context of serum protein analysis. You’ve evaluated Mitra® devices for microsampling of serum because transporting dried bio-fluids on Mitra has economic and logistical advantages over typical liquid sampling. Can you briefly discuss your study on measurement of proteins in dried serum using Mitra, and what you learned?
Dr. Pennington: I’m happy to do that, but maybe before that I can summarize the studies that we’ve undertaken with serum on Mitra devices into some context. Atturos is developing advanced diagnostic tests that rely on the measurement of multiple proteins in serum. The measurements are made using a robust sample preparation workflow and a proteomics approach that uses mass spectrometry to specifically and sensitively measure a few hundred potential biomarkers simultaneously.
 We can do this using a few microliters of serum. I hope it becomes immediately apparent that that’s very compatible with the loading and capacity of the Mitra devices.
We can do this using a few microliters of serum. I hope it becomes immediately apparent that that’s very compatible with the loading and capacity of the Mitra devices.
While we’ve been developing these tests, it became apparent that the cost and the logistics associated with just getting a serum sample under temperature-controlled conditions to the laboratory is one of the most complex and challenging parts of the whole test workflow.
Of course, it also requires that those samples, as well as being shipped at -80°, go through customs and the problems that can entail. A number of years ago, we set up a collaboration with the Gemelli Hospital in Rome where they have a personalized medicine initiative.
In that collaboration, they took duplicate samples from their standard clinical diagnostics laboratory and sampled them onto Mitra devices. They did that by dipping the [absorptive VAMS®] tips into a serum sample. Those were dried and then posted to the Atturos laboratory.
That meant that compared to the dry ice shipping, it was a lot cheaper and quicker, and the samples didn’t go through customs. We then put those samples into the Atturos workflow. We made some minor modifications to the workflow, but we were subsequently able to show that the delivery of samples using Mitra devices provides for very reproducible assay results and stability.
We were really reassured to see that the serum samples stored on the Mitra devices were stable for up to six months. And now that they’re in the laboratory, of course, they don’t need the -80° freezers for storage, so storage is greatly simplified.
Neoteryx: Microsampling of capillary blood is another important application for Mitra devices, of course. These devices make it easy for people at home to perform remote blood collection by self-collecting their own microsamples from a tiny finger-prick. Can you discuss how remote microsampling can help participants in multi-center research studies, such as the HIPPOCRATES study?
Dr. Pennington: Before I do that, perhaps I can introduce HIPPOCRATES. It is an INNOVATIVE MEDICINES INITIATIVE (IMI) m funded project - a public-private partnership. HIPPOCRATES is specifically focused on psoriatic disease. The consortium comprises of 26 partners across Europe that includes four pharmaceutical companies, a number of SMEs including Atturos, and many of the major clinical centers that specialize in psoriatic arthritis throughout Europe.
It is funded to the tune of 21 million Euros and is a 5-year project that has just begun. It sets out to address unmet needs in psoriatic arthritis (PsA). This is a form of arthritis associated with the skin disease psoriasis. Around 30% of patients with psoriasis will go on to develop psoriatic arthritis. One of the issues at the moment is that we don’t know which of the patients with psoriasis will go on to develop psoriatic arthritis.
And, very often, because those patients are seen in a dermatology clinic, their musculoskeletal symptoms are not picked up early enough.
So, there is a real unmet need to be able to identify patients with psoriasis who progress to psoriatic arthritis. An aspiration is to be able to predict which patients with psoriasis will develop psoriatic arthritis, because that gives you the opportunity to do something that almost all clinicians would like to be able to do, which is to be able to prevent a disease.
So, if you could predict which patients with psoriasis will go on to develop psoriatic arthritis, you have at least the opportunity to prevent that progression in a group of patients.
One of the work packages in HIPPOCRATES — it’s divided into eight work packages — focuses specifically on our ability to predict PsA before it develops. As part of this work package, we have the very ambitious HIPPOCRATES Prospective Observational Study (HPOS). The aim of which is to recruit 25,000 patients across Europe who have psoriasis and then follow them longitudinally.
From existing data, we know that that around 600 of these patients per year will develop PsA. This study is web-based, and participants will provide completed patient-reported questionnaires, and we also want to be able to sample some of them. Within HIPPOCRATES we have provision for sampling 2,500 of the patients to take a finger-prick blood sample.
Clearly, the costs of having those patients come into a clinic for a phlebotomy blood draw would prohibitive.
We’re going to sample 2,500 patients and the intention is that whole blood samples will be used for genomic SNP analysis. It turns out that although HPOS, even as it stands is, ambitious, a number of the participants of the consortium and have got really excited about the opportunity to extend that study whereby we might sample all 25,000 patients.
We’d not just sample them for whole blood, but maybe identify a way of sampling them for serum or plasma. That will only be logistically possible if those patients provide the sample themselves rather than going into a hospital and having it done through a standard venous blood draw and serum sample preparation.
The pharma companies are involved, and others have got very excited about that because it addresses some of their issues around clinical trials, which is making sure that their recruitment to those clinical trials captures people who may be in more remote locations or who are currently living in underserved populations. I think the patient-centric sampling approach really does provide for that more inclusive, broader net-casting.
Neoteryx: I think with the COVID-19 pandemic, the patient-centric sampling has become more vital, and the HIPPOCRATES study that you just outlined, and HPOS within that, is going to demonstrate the importance of this type of sampling. How do you foresee remote microsampling advancing the field of proteomics and personalized medicine?
For example, do you anticipate more scientists adopting microsampling as they discover they can develop excellent assays and tests with smaller sample sizes? And do you expect more scientists will support the use of microsampling where it can help personalized medicine programs—for patient comfort, for example, and for the other advantages it offers?
Dr. Pennington: Do I foresee more scientists using it? I think where the sample size that you can get on a Mitra device is compatible with the kinds of assays that the scientists might be working with then, yes, I do.
But, as you know, one size doesn’t fit all, and there will be applications for which the sampling isn’t compatible with the volume or even the approach used for particular technologies.
We’re very fortunate because it is compatible with mass spectrometry. That has been our immediate experience. It may be less compatible with affinity-based proteomics approaches that may rely on or have relied on the conformation of the protein being similar or close enough to a native serum sample to a frozen and thawed serum sample.
That may not be the case for a dried sample, but everything has its limitations. Of course, we’re excited by the possibility that the microsampling is now compatible for blood, serum and plasma. I think you’re right about the COVID-19 pandemic.
I think it has heralded a new era in healthcare provision, particularly telemedicine. I was at a meeting in the UK last week where [it was clear that] within the healthcare system in the UK telemedicine has become more acceptable, whereas a few years ago it was strongly resisted.
Now all the benefits of it are being seen. I think the missing piece, as you alluded to, is that telehealth and remote monitoring consultations can be held but getting access to the associated clinical data to support the consultation can be challenging and has been challenging when patients haven’t been able to go into hospital to have a blood draw, or now may not want to go into a hospital because they perceive it as being too risky.
We see benefit in a workflow in which the patient provides the sample at home, and it gets sent to a testing laboratory to get really reliable diagnostic test data that supports these telemedicine consultations that patients may have with their physicians.
Therefore, the advantage of patient-centric sampling might not be so much in patient comfort, but in patient convenience. The reduced need for making those phlebotomy appointments, taking time off work, traveling to go and have a blood draw.
We heard in this meeting last week that some patients in London have to take a day of work to get to hospital to have a venous blood draw. So, to be able to do that at home is hugely beneficial! I suppose the issue, and this has been reported, is that there is still not clear concordance between data that is generated from a sample taken in the regulated environment of a hospital compared to a sample that is taken at home.
As you know, whilst pharmaceutical companies have engaged with the use of patient-centric sampling to support their clinical trials, I think for widespread adoption in clinical trials and the general healthcare setting, there is going to need to be a demonstration that there is equivalence between the test results obtained from a sample taken at home to a sample taken in a more regulated environment. In that context, we’re excited that we’ve begun a new project funded by the Irish Government.
It’s called “Persona,” and will provide a personalized, patient-centric sampling workflow. We will try to bring together Neoteryx® Mitra® microsampling devices that Trajan provides with automated sample preparation workflow from Agilent Technologies. We’ll be interfacing theses with the advanced diagnostic tests that Atturos are developing, and collaborating with UCD’s Clinical Research Centre to align with more routine tests that are used in existing clinical diagnostic testing. I think it’s that kind of data that will really see the increased adoption of this new pathway of getting samples conveniently, and perhaps for some patients more comfortably, taken in their own home.
Neoteryx: What do you see as the greatest hurdle to the adoption of proteomic / other omic assays such as metabolomic and/or genomic. How do you see these hurdles being overcome?
Dr. Pennington: I think that COVID-19 has clearly been a very negative experience globally, but the positive is that it has driven the impetus to move forward on these remote sampling initiatives. As we move forward, the brilliant minds that can be brought to play mean that the hurdles will be overcome. I don’t have a sufficiently brilliant mind to be able to identify how they’ll be overcome, I’m just confident that they will be!
Of course, our focus is on proteomics applications. I don’t doubt that there will be benefit to metabolomics and genomics applications, and that they’ll have a very significant impact. [In proteomics, for us] the biggest hurdle is how you go from sampling a finger-prick of blood to generating a plasma-like or serum-like sample at home.
Clearly, that increases our chances of doing these proteomics measurements. We can do measurements on whole blood, but it presents challenges in terms of the bulk of that sample being a series of proteins that we are not particularly interested in measuring. They mask the measurement of the proteins that we are interested in.
Blood, while suitable for many clinical tests, isn’t suitable for many existing tests –in our hands its not suitable for the multi-protein diagnostic tests that we are developing. I suppose that’s one hurdle — is to get device for patient-centric serum-like or plasma-like sampling. And I know that huge efforts and initiatives are being made to develop a next generation of sampling devices that can do that.
And, as you know, the Patient-Centric Sampling Working Group, which is part of the International Consortium for Innovation and Quality in Pharmaceutical Development, have noted the issues around getting data that demonstrates that the samples are appropriate, stable and they generate data comparable to other approaches, such as a venous blood draw. I suppose we really need to see some studies that show that the data that’s generated is equivalent to the data generated from venous blood draws. That’s why we’re excited about the PERSONA project we’re doing, that seeks to address the key data quality and workflow issues.
We really look forward to seeing the benefits of patient-centric sampling realized. Those benefits include being able to] monitor diseases that are associated with episodic events, where sampling can happen at the time of an event. For example, asthma patients can sample during a bout of asthma rather than sampling in a phlebotomy clinic at a later point when they’re having a relatively good day.
In the cases of individuals with chronic diseases, they’re managed over a number of years, so the continued inconvenience of visiting a hospital becomes very burdensome, which may also account for some drop off in patient compliance.
We also know that there are very vulnerable and at-risk populations for whom going to a hospital is challenging — [individuals who are] elderly, immunocompromised, or contagious — where going into a public setting endangers them and potentially others. I think [patient-centric sampling] also gives the opportunity for more frequent assessment of biomarkers.
If I’m getting really excited about the future of personalized medicine, that [would be a future] where a patient might be able to take a sample on a weekly basis, or even a daily basis, that provides a stable healthcare record. It may not even be analyzed at that time, but it is there as a diary of their healthcare status that one could go back to.
That would be really important for markers that have got a temporal component. There are huge advantages and potential for incorporating patient-centric sampling into the personalized medicine and healthcare of the future.
Neoteryx: Yes, patient-centric sampling really does have quite a bright future. Thank you, Dr. Pennington, for speaking with us about how you apply microsampling in your proteomic work. We wish you great success with your studies and other projects!
More About Dr. Pennington: https://people.ucd.ie/stephen.pennington/publications
Explore our Microsampling in Omics resource page for additional information:

Image Credits: University College Dublin, Trajan, Neoteryx, iStock
Share this
- Microsampling (206)
- Research, Remote Research (119)
- Venipuncture Alternative (105)
- Clinical Trials, Clinical Research (83)
- Mitra® Device (73)
- Therapeutic Drug Monitoring, TDM (51)
- Dried Blood Spot, DBS (39)
- Biomonitoring, Health, Wellness (30)
- Infectious Disease, Vaccines, COVID-19 (24)
- Blood Microsampling, Serology (23)
- Omics, Multi-Omics (21)
- Decentralized Clinical Trial (DCT) (20)
- Specimen Collection (18)
- Toxicology, Doping, Drug/Alcohol Monitoring, PEth (17)
- Skin Microsampling, Microbiopsy (14)
- hemaPEN® Device (13)
- Preclinical Research, Animal Studies (12)
- Pharmaceuticals, Drug Development (9)
- Harpera Device (7)
- Industry News, Microsampling News (5)
- Antibodies, MAbs (3)
- Company Press Release, Product Press Release (3)
- Environmental Toxins, Exposures (1)
- July 2025 (1)
- May 2025 (1)
- April 2025 (2)
- December 2024 (2)
- November 2024 (1)
- October 2024 (3)
- September 2024 (1)
- June 2024 (1)
- May 2024 (1)
- April 2024 (4)
- March 2024 (1)
- February 2024 (2)
- January 2024 (4)
- December 2023 (3)
- November 2023 (3)
- October 2023 (3)
- September 2023 (3)
- July 2023 (3)
- June 2023 (2)
- April 2023 (2)
- March 2023 (2)
- February 2023 (2)
- January 2023 (3)
- December 2022 (2)
- November 2022 (3)
- October 2022 (4)
- September 2022 (3)
- August 2022 (5)
- July 2022 (2)
- June 2022 (2)
- May 2022 (4)
- April 2022 (3)
- March 2022 (3)
- February 2022 (4)
- January 2022 (5)
- December 2021 (3)
- November 2021 (5)
- October 2021 (3)
- September 2021 (3)
- August 2021 (4)
- July 2021 (4)
- June 2021 (4)
- May 2021 (4)
- April 2021 (3)
- March 2021 (5)
- February 2021 (4)
- January 2021 (4)
- December 2020 (3)
- November 2020 (5)
- October 2020 (4)
- September 2020 (3)
- August 2020 (3)
- July 2020 (6)
- June 2020 (4)
- May 2020 (4)
- April 2020 (3)
- March 2020 (6)
- February 2020 (3)
- January 2020 (4)
- December 2019 (5)
- November 2019 (4)
- October 2019 (2)
- September 2019 (4)
- August 2019 (4)
- July 2019 (3)
- June 2019 (7)
- May 2019 (6)
- April 2019 (5)
- March 2019 (6)
- February 2019 (5)
- January 2019 (8)
- December 2018 (3)
- November 2018 (4)
- October 2018 (7)
- September 2018 (6)
- August 2018 (5)
- July 2018 (8)
- June 2018 (6)
- May 2018 (5)
- April 2018 (6)
- March 2018 (4)
- February 2018 (6)
- January 2018 (4)
- December 2017 (2)
- November 2017 (3)
- October 2017 (2)
- September 2017 (4)
- August 2017 (2)
- July 2017 (4)
- June 2017 (5)
- May 2017 (6)
- April 2017 (6)
- March 2017 (5)
- February 2017 (4)
- January 2017 (1)
- July 2016 (3)
- May 2016 (1)
- April 2016 (2)

No Comments Yet
Let us know what you think