Share this
microsampling to map a pandemic: Kaitlyn Sadtler, PhD
by Neoteryx Microsampling on Nov 6, 2023 9:00:00 AM
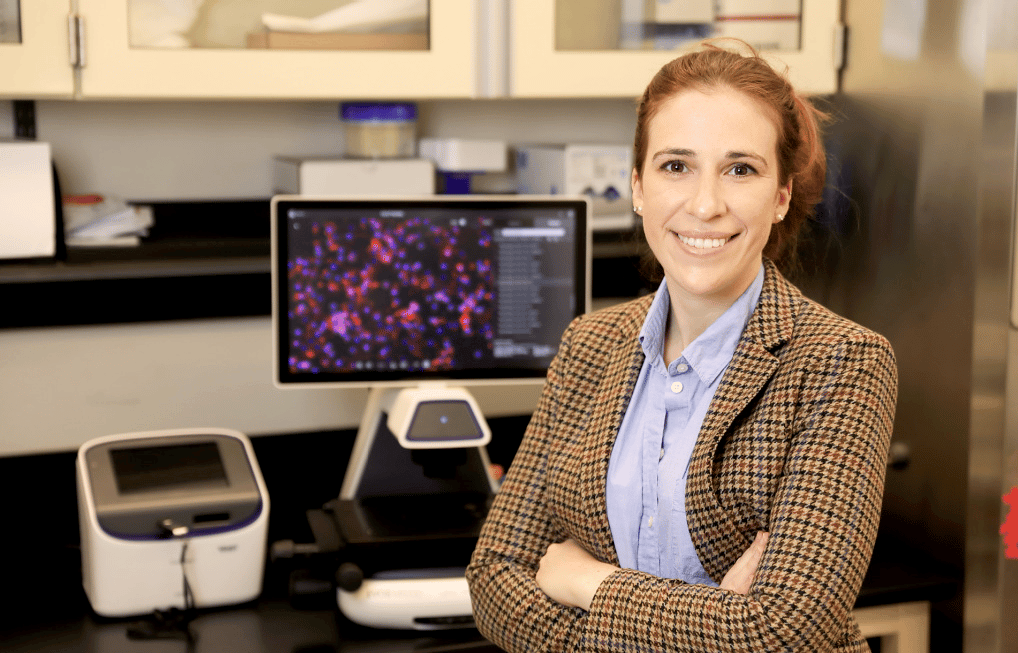
For this episode of the Microsamplify Podcast, we spoke with research scientist Kaitlyn Sadtler, PhD, an Earl Stadtman Tenure-Track Investigator and Chief of the Section for Immunoengineering at the National Institute of Biomedical Imaging and Bioengineering (NIBIB), part of the National Institutes of Health (NIH).
In early 2020, Dr. Sadtler and a team of researchers conducted one of the very first serology studies of the novel coronavirus known as SARS-CoV-2, in an effort to identify undetected cases of COVID-19 illness in the United States.
The study discussed in this podcast is a collaborative, multi-center effort. Dr. Sadtler and her research section team at NIBIB would like to acknowledge the invaluable contributions made by their research collaborators and co-investigators at NIAID (Dr. Matthew Memoli), NCATS (Dr. Matthew Hall), FNLCR (Dr. Dominic Esposito) within the NIH, and also at the University of Pittsburgh (Dr. Steven Reis) and the University of Alabama at Birmingham (Dr. Robert Kimberly).
Neoteryx: Hello Dr. Sadtler, and welcome to the Microsamplify Podcast from Neoteryx. Thanks for taking the time to speak with us about your work at NIBIB in Bethesda, Maryland.
Dr. Sadtler: Thank you so much for having me.
Neoteryx: I know that immunology is the general focus of your research, and that you aim to use laboratory methods that are translatable to the medical arena, but can you tell us a little more about yourself, and give us an overview of your broad research interests in immunology, regenerative medicine, tissue engineering and foreign body response at NIBIB?
Dr. Sadtler: I started off in basic immunology, meaning understanding how our immune system reacts to different stimuli like bacteria and viruses, and generally how the cells behave in our body. After that, I moved into the world of tissue engineering and regenerative medicine, where the goal is to grow back missing or damaged tissue.
Since then, I’ve been working in kind of that intersection between basic immunology and biomedical engineering. The immune system is really a richly complex network of immune cells and proteins that can affect any process in our body—from the obvious, like defending us against infections like SARS-CoV-2, to the less obvious, like helping neurons form new connections with each other.
It takes in information from the organ that its acting in, from our own genetics, and even information from the friendly bacteria that live within our bodies. And it creates a specific response to a given stimuli. For our lab, the stimuli that we are investigating are medical device implants and trauma.
The immune system can determine whether or not that cut on your arm gets replaced by functional new tissue full of hair follicles and sweat glands, or if it turns into a big scar. And the same is true in other tissues, like muscle, which is one of our focuses. In regenerative medicine, our goal is to grow back new tissues that are lost due to damage, disease or genetic mutations.
We can’t do that without first understanding our immune system.
Neoteryx: On your Section for Immunoengineering website it states that your lab, “develops immune-active biomaterials for regenerative medicine through a bottom-up approach using mechanism-based immunology methods.” Can you share with us your current research in this area before your priorities shifted to COVID-19?
Dr. Sadtler: As I mentioned previously, we really can’t start to approach therapeutics for tissue engineering and the replacement of damaged organs until we understand the way our immune system interacts with the materials we’ve engineered and devices that are used to reconstruct these damaged tissues.
So, for muscle injury, we can put a material into a wound that beautifully recapitulated [replicated] that muscle structure when it was outside the body. But once we put it inside the body, it would create a massive amount of inflammation, causing more harm to that already damaged area.
On the other hand, we could put in a material that causes severe scar formation, and instead of functional tissue, we just get that giant scar. Therefore, if we understand how our immune system interacts with materials that create environments that are conducive to wound healing and regeneration, we can leverage this understanding to create targeted therapeutics that regrow tissue by modulating our immune system.
Neoteryx: So let’s turn now to COVID-19. Starting in April 2020, as the coronavirus pandemic was gaining momentum, you and your colleagues at the NIH collectively and rapidly developed a serological assay specific to SARS-CoV-2.
You and your co-investigators have since published a paper in Nature Communications on your dual-antigen ELISA protocol that evaluates IgG and IgM antibodies against both the spike ectodomain and the RBD. Can you discuss this SARS-CoV-2 protocol and how you maximize throughput and reproducibility to be able to process thousands of samples?
 Dr. Sadtler: The SARS-CoV-2 “Sero-Survey” work is an example of inter-institute collaboration within the NIH.
Dr. Sadtler: The SARS-CoV-2 “Sero-Survey” work is an example of inter-institute collaboration within the NIH.
Along with NIBIB, we also worked with the National Institute of Allergy and Infectious Diseases (NIAID), the National Center for Advancing Translational Sciences (NCATS), and the Frederick National Laboratory for Cancer Research (FNLCR).
So, with those different groups, what we focused on was relying on first optimizing the different antigens used for antibody detection. We didn’t want to reinvent the wheel, so we tested constructs that existed from other groups that were kind enough to send them over to us. We found two of these antigens worked the best, in terms of both feasibility and producing the protein itself.
And, of course, the signal-to-noise ratio on the ELISA, which is the platform we use. And, special thanks to the NIAID Vaccine Research Center and Dr. Jason McClellan for that spike construct, as well as Dr. Aaron Schmidt from the Ragon Institute for the RBD construct.
Using both of those allowed us to have a heightened sensitivity and specificity that was not possible with just one antigen alone. This sensitivity and specificity are really critical when evaluating thousands of samples. Furthermore, in addition to using clinically derived patient convalescent blood samples—blood from people that we know have had SARS-CoV-2—we utilized recombinant monoclonal antibodies against the spike protein.
These are commercially available and are precise and in a controlled concentration. We won’t run out of them. If somebody wants to compare their data to ours directly, they can run a standard curve of those antibodies instead of using patient-derived samples that can run out, and are not known to be of an absolute concentration of an antibody.
Also, using blood samples taken before the pandemic started, we’re able to show the stability of the assay and really minimize false positive readings, allowing us to be really confident in our data. And when we applied this to a semi-automated robotic setup, we were able to increase that throughput while maintaining precise control of the assay.
Neoteryx: On the practical side, how were you able to collect thousands of samples over the sampling period of 11-weeks from study volunteers across the US? Can you share with us how you overcame the hurdles of obtaining nearly 9,000 blood samples during a pandemic when stay-at-home restrictions were firmly in place?
Dr. Sadtler: Quite a lot of these serologic studies utilize retrospective samples—samples that already existed from things such as routine bloodwork or dialysis. Our goal was to go out and collect samples, which has that added bit of complexity. This is where dried blood sampling really came into play.
In general, we knew we couldn’t bring everyone into a clinic during a respiratory virus pandemic, especially early on when transmission dynamics were poorly understood. So using remote sample collection and shelf-stable samples like dried blood, we were able to reach quite far away, geographically speaking.
Also, being a remote collection means that individuals didn’t need to have a clinic nearby [in order] to donate blood. Because it’s really difficult if you want to volunteer in a study, but your closest clinic that is able to draw blood is an hour or two away.
Neoteryx: Can you discuss how this study, which used remote specimen collection kits and Mitra® microsampling devices with VAMS® technology, differs from your past projects or public health surveillance studies within the US?
Dr. Sadtler: Dried blood sampling has been used previously in public health studies. Our goals here were to collect a representative sample of the United States, and that was really only possible using remote collection.
Being able to reach volunteers at their homes and not requiring a venipuncture blood draw was very important.
If you think about it in the context of other health monitoring, like for people with diabetes who prick their fingers daily to keep track of their blood sugar, can you imagine if that had to be venous blood?
So, practically speaking, at-home sampling [with a finger-prick method] was the way to go. This was one of the larger uses of dried blood sampling that we are aware of, especially considering the longitudinal aspect of our study.
Our study participants are collecting blood at three timepoints over the course of a year. We hope that this study provides an analysis pipeline that could be utilized to look at seroprevalence of other infectious diseases in the future.
Neoteryx: In what other types of studies or areas of research might microsampling be applicable, and is your lab planning for those types of studies in the future?
Dr. Sadtler: In my viewpoint, shelf-stable samples are a great avenue for research that covers things like a large geographic area, in our case, the United States. We got as far away as Alaska and Hawaii. And it helps reach more remote populations that don’t have quick access to a clinic, both in rural areas in the United States and in other countries as well.
You start to eliminate some of those cold-chain issues that pop up with samples of serum or plasma—where you need to keep them frozen down. We know that we can study antibodies using dried blood, and I think there are quite a few other stable analytes in the blood that could be viewed and evaluated as well.
There is plenty that can be done and, personally, I’m all about engineering approaches to healthcare. So remote sample collection really opens the door for studies that wouldn’t be feasible if they relied just solely on the clinic.
Neoteryx: Thank you, Dr. Sadtler, for speaking with us about how you and your group were the first to report on the prevalence of asymptomatic SARS-CoV-2 infection across a representative sample of people within the US. We wish you and your colleagues great success with your follow-up studies!

Image credit: NIH photos by Chia-Chi Charlie Chang
Share this
- Microsampling (206)
- Research, Remote Research (119)
- Venipuncture Alternative (105)
- Clinical Trials, Clinical Research (83)
- Mitra® Device (73)
- Therapeutic Drug Monitoring, TDM (51)
- Dried Blood Spot, DBS (39)
- Biomonitoring, Health, Wellness (30)
- Infectious Disease, Vaccines, COVID-19 (24)
- Blood Microsampling, Serology (23)
- Omics, Multi-Omics (21)
- Decentralized Clinical Trial (DCT) (20)
- Specimen Collection (18)
- Toxicology, Doping, Drug/Alcohol Monitoring, PEth (17)
- Skin Microsampling, Microbiopsy (14)
- hemaPEN® Device (13)
- Preclinical Research, Animal Studies (12)
- Pharmaceuticals, Drug Development (9)
- Harpera Device (7)
- Industry News, Microsampling News (5)
- Antibodies, MAbs (3)
- Company Press Release, Product Press Release (3)
- Environmental Toxins, Exposures (1)
- July 2025 (1)
- May 2025 (1)
- April 2025 (2)
- December 2024 (2)
- November 2024 (1)
- October 2024 (3)
- September 2024 (1)
- June 2024 (1)
- May 2024 (1)
- April 2024 (4)
- March 2024 (1)
- February 2024 (2)
- January 2024 (4)
- December 2023 (3)
- November 2023 (3)
- October 2023 (3)
- September 2023 (3)
- July 2023 (3)
- June 2023 (2)
- April 2023 (2)
- March 2023 (2)
- February 2023 (2)
- January 2023 (3)
- December 2022 (2)
- November 2022 (3)
- October 2022 (4)
- September 2022 (3)
- August 2022 (5)
- July 2022 (2)
- June 2022 (2)
- May 2022 (4)
- April 2022 (3)
- March 2022 (3)
- February 2022 (4)
- January 2022 (5)
- December 2021 (3)
- November 2021 (5)
- October 2021 (3)
- September 2021 (3)
- August 2021 (4)
- July 2021 (4)
- June 2021 (4)
- May 2021 (4)
- April 2021 (3)
- March 2021 (5)
- February 2021 (4)
- January 2021 (4)
- December 2020 (3)
- November 2020 (5)
- October 2020 (4)
- September 2020 (3)
- August 2020 (3)
- July 2020 (6)
- June 2020 (4)
- May 2020 (4)
- April 2020 (3)
- March 2020 (6)
- February 2020 (3)
- January 2020 (4)
- December 2019 (5)
- November 2019 (4)
- October 2019 (2)
- September 2019 (4)
- August 2019 (4)
- July 2019 (3)
- June 2019 (7)
- May 2019 (6)
- April 2019 (5)
- March 2019 (6)
- February 2019 (5)
- January 2019 (8)
- December 2018 (3)
- November 2018 (4)
- October 2018 (7)
- September 2018 (6)
- August 2018 (5)
- July 2018 (8)
- June 2018 (6)
- May 2018 (5)
- April 2018 (6)
- March 2018 (4)
- February 2018 (6)
- January 2018 (4)
- December 2017 (2)
- November 2017 (3)
- October 2017 (2)
- September 2017 (4)
- August 2017 (2)
- July 2017 (4)
- June 2017 (5)
- May 2017 (6)
- April 2017 (6)
- March 2017 (5)
- February 2017 (4)
- January 2017 (1)
- July 2016 (3)
- May 2016 (1)
- April 2016 (2)

No Comments Yet
Let us know what you think