Share this
variances in DBS observed for neonatal screening
by James Rudge, PhD, Technical Director, Neoteryx on Nov 14, 2022 9:00:00 AM
An article published by SK Hall et al at three hospitals in the United Kingdom in the June 2015 issue of Journal of Medical Screening, reported on an investigation into biases seen with dried blood spot (DBS) sampling in newborn screening laboratories. The paper is entitled “Newborn screening blood spot analysis in the UK: influence of spot size, punch location and haematocrit.” It describes how the location of the punch on a DBS card, spot size and hematocrit all affect analytical data from biomarkers of inborn errors of metabolism and related conditions.
The research team was able to conclude that differences in blood spot size, hematocrit and punch location substantially affected measured concentrations for analytes used in the UK newborn screening program. They reported in their article that this could affect false positive and negative rates. The researchers proposed that to minimize analytical bias, “these variables should be controlled or adjusted for where possible.”
The Importance of Neonatal Screening
 Neonatal screening programs are vital to help identify metabolic disorders at birth so that treatment interventions can be initiated early to prevent progression of a disease or to manage the symptoms.
Neonatal screening programs are vital to help identify metabolic disorders at birth so that treatment interventions can be initiated early to prevent progression of a disease or to manage the symptoms.
There is currently a wide range of genetic and metabolic conditions that are screened for at birth, including congenital hypothyroidism, phenylketonuria, cystic fibrosis, Medium-chain acyl-CoA dehydrogenase deficiency (MCADD), and maple syrup urine disease (MSUD).
Since the early 1960s, early newborn screening has involved the collection of capillary blood, usually from a heel-prick, onto a DBS filter paper or card where the blood is dried and sent to a laboratory for tests.
The tests vary dependent on the condition being screened, but often they measure the build-up of a metabolite such as phenylalanine as observed in phenylketonuria patients. The DBS technique of collecting samples from newborns has eradicated the use of the more invasive and complicated venipuncture technique to collect blood.
Biases Seen with Dried Blood Samples
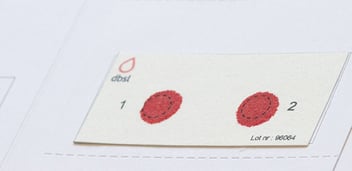 DBS cards have stayed the test of time in the microsampling industry, but there are several fundamental drawbacks of DBS technology that make it difficult to obtain high precision in analytical data. The primary reason for this is due to the way DBS cards are processed in the laboratory.
DBS cards have stayed the test of time in the microsampling industry, but there are several fundamental drawbacks of DBS technology that make it difficult to obtain high precision in analytical data. The primary reason for this is due to the way DBS cards are processed in the laboratory.
To attempt to obtain a volumetrically precise sample, DBS cards are ‘hole punched’ to obtain fixed diameter sub-punches. In neonatal screening for example, 3.2 mm punches are popular, which yields about 3 µL of blood at 45% hematocrit (HCT). However, HCT can vary in newborns (from ~30 -65%) and this can have deleterious effect on results. This is because the actual volume of blood collected from the sub-punch can be very misleading due to the following analytical biases:
- Spot spread bias – The higher the % of HCT, the more viscous the sample, which leads to smaller spot diameters for the same volume applied. The more enriched the fixed volume sub-punch is, the more often this leads to +ve biases.
- Punch location bias – This is where different values are seen for some analytes dependent on where the punch was taken.
- Extraction bias – This describes how the % HCT affects the extraction efficiency. Without method optimization, negative biases are often observed at higher % HCT levels. This can also be observed with volumetrically collected samples.
- Matrix bias – The greater the HCT level the greater the chance of matrix effects.
Another bias that can be observed, even if a fixed % HCT is applied, is spot area bias. This is because it is difficult to meter the volume of blood collected from a finger or heel directly to a DBS card so the actual diameter of the spot can vary the concentration of the analytes in the spot which, in turn, can bias the results.
To test the extent to which biases are observed in neonatal screening, SK Hall and co-authors of the study paper summarized here investigated to evaluate the following biases: spot spread bias, punch location bias, and spot area bias.
DBS Study Methods and Findings
- L-phenylalanine, L-methionine, L-tyrosine, L-leucine, Octanoylcarnitine (C8), human thyroid stimulating hormone (TSH), and immunoreactive trypsinogen (IRT) were measured from blood spots at different concentrations and at different HCT levels.
- To measure punch location bias and spot area bias, cards with increasing spot sizes were created by applying 10, 20, 50 and 75 µL for all spot sizes 30.2 µL sub-punches were taken in the middle of each spot. For 50 and 75 µL spots peripheral samples were also taken.
- To measure HCT bias, DBS were spotted with 50 µL samples of increasing %HCT concentrations (30, 40, 45, 50 and 60%) for all analytes except for IRT where the range was 25, 50 and 65%.
- To measure the heterogeneity of the blood samples based on size, light transmission was measured using a Cardscan™ system. The purpose of this was to see if there were differences in transmissibility levels dependent on the spot size and also on the location of the DBS paper, as well as impact of HCT level.
- In terms of spot size, a significant reduction (sometimes up to 20%) in measured analyte levels (except for IRT where only the lower concentration showed the effect) were observed when smaller volumes of blood were deployed (10 to 20 µL) compared to 50 and 75 uL.
- In terms of punch locations, measured analyte concentrations where significantly higher at the periphery of the blood spot (up to 35%) for all analytes tested.
- For the HCT measurement, increasing HCT values showed a reduction of TSH and C8 levels. However, for leucine, methionine, phenylalanine and tyrosine, the levels increased with increasing HCT. IRT showed a significant reduction (10-15%) at 65% HCT.
- In terms of light transmission, there was a reduced transmissibility with increasing spot size. Furthermore, transmission was significantly greater at the edge of the spots.
Study Authors’ Discussion and Conclusions
- Punch location can significantly affect the measured analyte concentration, which aligns with previous published studies. As a number of these analytes have greater fractions in plasma compared to intracellular fluid, this aligned with the edge data where transmissibility is higher.
- Analysis of spot diameter showed a decrease in analyte levels with decreasing spot size, suggesting that the smaller the volume of blood added to the filter card, the further the blood spreads.
- Observed increase in concentrations of leucine, methionine, phenylalanine, and tyrosine with increasing hematocrit may be due to HCT spread bias or changes in plasma volume.
- It may be more difficult to explain why some analytes decreased in concentration with increasing HCT, but it may be due to the way blood migrated in the card matrix.
- The results from spot size, punch location and differing HCT could lead to false positives and false negatives in the data. This occurs despite the fact that instructions are given to neonatal nurses and midwives to apply appropriate blood volumes to DBS cards from a heel prick. To a certain extent, labs can QC the spots and control punch locations to help mitigate these concerns.
- The authors proposed that the Cardscan™ could be used as a surrogate marker for punch location and HCT levels.
Comments from Neoteryx
The impact that DBS has had on early detection of genetic diseases and errors in metabolism in newborn babies cannot be underestimated. However, the fundamental issues associated with attempting to quantitate from DBS filter paper or cards, especially in a cohort where HCT can vary wildly, demanded some improvements in the field of blood microsampling.
The need to overcome the limitations of DBS cards created an opportunity in the microsampling industry for new sample-collection devices that offered a more precise volumetric approach to blood sampling. Indeed, the volumetric nature of newer sample collection tools such as hemaPEN® and Mitra® devices based on VAMS® technology have the potential to overcome many of the issues (spot size, punch location and HCT spread biases) observed in the work cited here.
/hemaPEN%20images%20(approved)/HP%20Illustration_DBScart_12x10-1.png?width=273&height=228&name=HP%20Illustration_DBScart_12x10-1.png) These new fixed-volume microsampling devices may offer a solution for current and next-generation newborn screening assays.
These new fixed-volume microsampling devices may offer a solution for current and next-generation newborn screening assays.
For example, the hemaPEN device offers end-users who are accustomed to using DBS cards with an easy transition to a next-generation precision DBS device. With a single heel-stick or finger-stick, the hemaPEN simultaneously collects 4 volumetrically identical (2.74 µL) blood samples via rapid capillary action.
Once the end-user has collected the samples and clicks the lid back onto the hemaPEN to shut it, those 4 samples are transferred onto 4 pre-cut DBS disks inside the device’s tamper-resistant housing. The hemaPEN now contains 4 blood spots of equal size with no HCT spread and is ready for delivery to the lab for DBS processing and analysis that eliminates the hole-punching step.
This article was summarized for our readers by James Rudge, PhD, Neoteryx Technical Director. This is curated content. To learn more about the important research outlined in this blog, visit the original article in the Journal of Medical Screening.
Image Credits: iStock, Neoteryx, Trajan

For more information on how Neoteryx microsampling products from Trajan help researchers, visit our Technical Resource Library.
Share this
- Microsampling (205)
- Research, Remote Research (118)
- Venipuncture Alternative (106)
- Clinical Trials, Clinical Research (82)
- Mitra® Device (72)
- Therapeutic Drug Monitoring, TDM (50)
- Dried Blood Spot, DBS (38)
- Biomonitoring, Health, Wellness (31)
- Infectious Disease, Vaccines, COVID-19 (24)
- Decentralized Clinical Trial (DCT) (22)
- Blood Microsampling, Serology (21)
- Omics, Multi-Omics (19)
- Specimen Collection (17)
- Toxicology, Doping, Drug/Alcohol Monitoring, PEth (17)
- hemaPEN® Device (13)
- Preclinical Research, Animal Studies (12)
- Pharmaceuticals, Drug Development (9)
- Harpera® Tool (5)
- Industry News, Microsampling News (5)
- Skin Microsampling, Microbiopsy (5)
- Company Press Release, Product Press Release (4)
- Antibodies, MAbs (3)
- Environmental Toxins, Exposures (1)
- April 2024 (3)
- March 2024 (1)
- February 2024 (2)
- January 2024 (4)
- December 2023 (3)
- November 2023 (3)
- October 2023 (3)
- September 2023 (3)
- July 2023 (3)
- June 2023 (2)
- April 2023 (2)
- March 2023 (2)
- February 2023 (2)
- January 2023 (3)
- December 2022 (2)
- November 2022 (3)
- October 2022 (4)
- September 2022 (3)
- August 2022 (5)
- July 2022 (2)
- June 2022 (2)
- May 2022 (4)
- April 2022 (3)
- March 2022 (3)
- February 2022 (4)
- January 2022 (5)
- December 2021 (3)
- November 2021 (5)
- October 2021 (3)
- September 2021 (3)
- August 2021 (4)
- July 2021 (4)
- June 2021 (4)
- May 2021 (4)
- April 2021 (3)
- March 2021 (5)
- February 2021 (4)
- January 2021 (4)
- December 2020 (3)
- November 2020 (5)
- October 2020 (4)
- September 2020 (3)
- August 2020 (3)
- July 2020 (6)
- June 2020 (4)
- May 2020 (4)
- April 2020 (3)
- March 2020 (6)
- February 2020 (3)
- January 2020 (4)
- December 2019 (5)
- November 2019 (4)
- October 2019 (2)
- September 2019 (4)
- August 2019 (5)
- July 2019 (3)
- June 2019 (7)
- May 2019 (6)
- April 2019 (5)
- March 2019 (6)
- February 2019 (5)
- January 2019 (8)
- December 2018 (3)
- November 2018 (4)
- October 2018 (7)
- September 2018 (6)
- August 2018 (5)
- July 2018 (8)
- June 2018 (6)
- May 2018 (5)
- April 2018 (6)
- March 2018 (4)
- February 2018 (6)
- January 2018 (4)
- December 2017 (2)
- November 2017 (3)
- October 2017 (2)
- September 2017 (4)
- August 2017 (2)
- July 2017 (4)
- June 2017 (5)
- May 2017 (6)
- April 2017 (6)
- March 2017 (5)
- February 2017 (4)
- January 2017 (1)
- July 2016 (3)
- May 2016 (1)
- April 2016 (2)


No Comments Yet
Let us know what you think